Food And Mood Connection and the happiness gut connection – Did you know that happy foods lead to happy moods via a happy gut?
Mental health problems are on the rise. More and more people are feeling stressed, anxious, depressed, or suffering from a diagnosed mental health condition, such as bipolar disorder or schizophrenia. According to Lancet (2018), almost 265 million people suffer from depression globally, while the figure for anxiety disorders is even higher at 284 million.
I myself see this in practice too. People who come to my clinic often suffer from anxiety and depression (alongside a not-so-happy gut) and are on antidepressant drugs. Also, the Food and Mood course that I run at the local Stepping Stones Recovery College Bracknell has turned out to be a very popular course, as people who suffer from various mental health issues are keen to understand food and mood connection and to learn how to manage their mental health better.
Drug therapy is the most commonly used intervention, alongside talking therapies (CBT), on the NHS in the UK. But too often, waiting lists to see a CBT therapist can be long, and often only a few sessions are offered, and many are then left taking their antidepressants long-term. A large proportion of people also fall through the cracks and never get any support.
What actually is going on?
Why are mental health issues so widespread these days?
The Covid pandemic had a lot to answer for, for sure!
According to a British government report ‘Wellbeing and mental health: Applying All Our Health’, from February 2022, self-reported mental health and well-being (including anxiety, stress, and depression) worsened during the pandemic and still remain worse than pre-pandemic levels.
The latest pre-pandemic (2019) results from Britain’s Healthiest Workplace Survey which included over 180,000 employees across the nation, showed that 1 in 10 people are living with depression. They also looked at stress, sleep, exercise, and diet, and found that 57% are stressed at work, 50% have money worries, 42% don’t sleep well, 1 in 3 don’t exercise enough and 65% are not eating a healthy diet. All factors affect mental health and need to be considered when treating mental health issues! I’m very keen to see how the post-pandemic results compare with these when they come out.
The Food and Mood Connection
For me as a nutrition and lifestyle medicine practitioner and a bit of a happy gut health geek, who strives for everyone to have a happy gut, there’s a crucial everyday link that we constantly tend to forget or quickly brush off. One that is far easier to manipulate and take control of by individuals themselves, even before one reaches for that prescription.
Your daily diet!
Your daily diet, unsurprisingly, delivers the building blocks not only for your physical but also for your mental health. The food you eat (the happy gut) has a big impact on your mood! Food and Mood connection!
Research shows the crucial importance of a healthy diet for the brain and mental health and the food and mood connection. There’s evidence to show how a highly refined, high-sugar, high-additive, ultra-processed diet is linked to low mood, addiction, and mental health issues. The detrimental effects happen via several mechanisms, including activation of brain reward centers, blood sugar imbalance, compromise the digestive function and gut health, and the effects on the immune and nervous systems.
Let’s take a look at the main mechanisms individually and then talk about how you can make small practical changes in your diet to make a difference in how you feel.
Addicted to sugar and processed foods?
The modern Western diet is by no means depleted of macronutrients, particularly carbohydrates and fats, or energy. We get plenty of these from our diet. But it’s not really hitting the mark when it comes to micronutrients (vitamins and minerals), phytonutrients (beneficial plant chemicals), and fibre.
We can safely say there’s quantity over quality in many people’s diets. Processed and packaged manufactured foods do not deliver the quality and nutrients that our bodies and brains need, but they are very easy to eat and can lead to overeating and addiction.
Processed foods are hyper-palatable foods created using a very precise food industry formula to achieve what’s referred to as the ‘bliss point’, which Wikipedia defines as “neither too much nor too little, but the “just right” amount of saltiness, sweetness, or richness.”
Other terms used in this context are ‘snackability’ and ‘craveability’, terms that make much sense if you’ve ever been in a situation when you just can’t put down that bag of crisps you started, can’t resist eating the whole packet of biscuits in your cupboard, or the bar of chocolate you bought on your way to work is calling your name from your desk drawer.
“Carbs are delicious, but they become deadly when the fibre is refined out.”
–The Psychobiotic Revolution (Scott C. Anderson, with John F. Cryan &Ted Dinan)

The food industry knows how to exploit a feature from human evolution – us humans evolved to favor foods that deliver these tastes. This may have given our ancestors a survival advantage in the days when food was scarce, and our ancestors had to endure periods of famine.
However, in today’s 24/7 society, when almost any type of fast-food meal is only a quick phone call away, this is no more advantage. The formula the food industry has developed makes us desire more, buy more and eat more of these kinds of foods. These flavors and the precise ratio of them, carefully thought through by the food scientists in white lab coats, hit the brain reward circuits that respond by secreting endorphins, dopamine, and other feel-good chemicals again pointing towards a food and mood connection.
And the pleasure you get from this is so good that, when enjoyed on a regular basis, your brain is telling you to have more and more to get that same hit again. A dopamine-seeking behavior, or in other words, addiction has been triggered!
The addictive nature of these kinds of foods has been shown in both animal and human studies. In rats, overconsumption of palatable food triggered addiction-like responses in brain reward circuits, driving compulsive eating. A study with 120 university students demonstrated that foods are not equal in how they affect our eating behaviors.
Food addiction seems to be a measure of food processing, the more processed and higher carb, the more likely a food is to lead to addiction. The researchers proposed parallels between the pharmacokinetic properties of recreational drugs and highly processed foods.
A famous rat study from 2007 also showed that when rats were allowed to freely choose between saccharin- (calorie-free sweetener) or sucrose- (normal table sugar) sweetened water and intravenous cocaine, the large majority of animals (94%) preferred the sweet-tasting water. You might think, that rats’ brains surely are different from our human brains… They are but maybe not that much, it seems.
A 2017 narrative review in the British Journal of Sports Medicine, stated that the evidence from the literature shows, in both animals and humans, substantial parallels between drugs of abuse and sugar, “from the standpoint of brain neurochemistry as well as behavior”.
So, what’s the takeaway from these studies?
The more you eat hyper-palatable processed foods and sugar, the more you want them! And the more you eat, the more you also need every time, in order to get that same hit of pleasure.
Furthermore, a regular or overconsumption of processed foods is a quick recipe for cravings, blood sugar spikes and crashes, energy and mood fluctuations, irritability, and that ‘hangry’ feeling, when nothing else does but another hit with these kinds of foods before you can be sociable again with people around you!
But this will keep you on a blood sugar rollercoaster ride that is nothing like the fun you get from that at an amusement park! It’s nothing but a recipe for a health disaster.
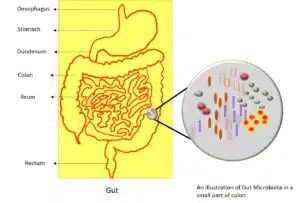
Food And Mood Connection -Your Gut is talking to Your Brain
As we saw from the studies mentioned above, your taste buds send messages to your brain – about the foods, or flavors you eat – to create a response in the brain. And so does your gut, not about the flavors but about everything that happens inside the gut! Your gut microbiome is in constant communication with your brain.
“Your gut is not like Las Vegas. What happens in the gut, does not stay in the gut!”
–Alessio Fasano, medical doctor, pediatric gastroenterologist, and gut researcher
The gut-brain axis is a hot topic in scientific literature so let’s have a look at it in more detail.
How are the gut and brain connected? The gut-brain axis consists of communication between the gut and the brain via several pathways:
Neurological –
The vagus nerve, your bidirectional communication highway between these two organs, as well as the gut’s own, ‘enteric’, nervous system, is linked to the central nervous system.
Immunological –
The crosstalk between the gut microbes and the immune cells.
Metabolic –
The compounds produced by the microbes include neurotransmitters serotonin, dopamine, and GABA, as well as beneficial anti-inflammatory short-chain fatty acids.
Endocrine –
The HPA (hypothalamus-pituitary-adrenal) axis, or the ‘fight or flight’ stress response.
We’ll look at each of these pathways in a minute. But first, a quick note about what kinds of things affect your gut.
Apart from your diet (which is huge!), your gut is also affected by (not an exhaustive list):
- Stress
- Sleep
- Alcohol
- Exercise
- Nature/Environment
- Mindset
- Medications (particularly antibiotics and acid-blocking drugs)
- Toxins
- Mode of delivery (vaginal/cesarean)
And the list goes on!
To have a happy gut, you need to reduce some of these exposures while increasing others. But with so many factors affecting your gut, you can feel reassured that there’s always something that you can do to make a difference, however small a change it is!
You don’t have to change everything from the get-go, just making small changes (or just one change) in any of the areas above can make a big difference in your gut health, mental health, and overall health. So, just focus on one small change at a time to start creating your happy gut.
So let’s have a look at the different gut-brain axis pathways.
The Neurological Pathway & The Vagus Nerve
Your gut is connected to your brain via a long nerve, the vagus nerve, the main nerve of the parasympathetic nervous system that controls the rest and digest response to calm your body after a stressful situation, or the fight or flight response. It delivers constant messages from the gut to the brain and from the brain to the gut.
What’s interesting is that it’s now understood that 90% of this communication is, in fact, “upwards traffic”, i.e. most messages are sent by the gut and received by the brain, and only 10% is coming down from the brain to the gut.
So, to keep your brain and moods happy, you have to have a happy gut! If it isn’t, your brain will get the message! The good news is that you can take control of the quality of this upward traffic by looking after the tiny microbes that call your gut home!
Your gut is your second brain!
Want a happy second brain? That is, a happy gut?
Then read on until the end for my tips!
You probably have at some point in your life had a “gut feeling” or felt “butterflies in your stomach”. That’s because your gut has an extensive network of nerve cells that form the gut’s own nervous system. This is called the enteric nervous system and is connected to the central nervous system. It has five times more neurons than your spinal column, which shows that your gut really is a feeling organ – your second brain!
The Immunological Pathway and the Microbe- Immune System Crosstalk
Your gut microbes play a crucial role in regulating your immune system. Signals derived from the gut microbiome are critical for the development of the immune system and maintaining an optimal immune function, essentially shaping and maintaining homeostasis of the immune system.
The various immune cells protect you from invaders, such as bacteria, viruses, and other pathogens and infectious agents. Your digestive tract, or gut, is the main interface between the inside of your body and the outside world. This is an important fact, in order to understand why 70% of your immune cells actually reside in and around the gut, ready to leap into action if anything harmful gets through from the outside, via the digestive system.
For a balanced immune system, the cells need to be able to differentiate between the harmful and harmless, or when to react and when to tolerate. Your microbes produce signaling molecules that serve as messages for the immune cells, educating the immune system about what is going on in the gut. When things are not well inside the gut, and when the intestinal barrier function is compromised (“leaky gut”), the immune cells get to work by mounting an immune response and secreting proinflammatory mediators.
These pro-inflammatory molecules can spread to any part of your body, including the brain. Inflammation can increase the permeability of the blood-brain barrier, allowing for easier entry of inflammatory molecules and immune cells into the central nervous system.
Current research supports the hypothesis that increased immune system activation is associated with depression and fatigue. Also, the prevalence of depression and anxiety is high in patients with diseases that involve immune activation, such as autoimmune disorders. Furthermore, antidepressant medication works less efficiently when there is low-grade inflammation present in patients with depression.
The Metabolic Pathway and Neurotransmitters
The microbes in the gut have many jobs. Not all the food you eat is digested by you or broken down by your digestive system, some compounds from your meals stay undigested and unabsorbed and travel to your colon, or large intestines, to feed the trillions of probiotic bacteria that reside there. This is your gut microbiome. As the bacteria feed on these compounds, they produce numerous health-promoting compounds or metabolites, that can affect the health of your gut, your body, and your brain.
Prebiotic compounds from the food you eat are like fertilizers for the probiotic microbial garden of your gut!
Some of these metabolites are anti-microbial substances that can protect you from harmful invaders, such as infectious agents. Some are anti-inflammatory molecules, such as the short-chain fatty acid butyrate, that not only help keep your gut lining healthy but also protect the brain from inflammation and increase neuroplasticity.
All this is good news for your moods too! But wait… there’s more!
Some neurotransmitters, or “brain chemicals” that are very important for you to feel happy and calm, are also produced by the gut microbiome, or your “happy gut” microbes. They are responsible for producing 95% of serotonin, your “happy hormone”, linked with depression (serotonin is a target of anti-depressant SSRI drugs). They also make dopamine which helps you feel motivated and find pleasure in life, and GABA, a calming neurotransmitter that opposes the fight or flight response and helps you sleep better.
And if that wasn’t enough, the probiotic bacteria also synthesize many vitamins such as vitamin K and some B vitamins, and by keeping the gut environment and lining healthy, they support the optimal absorption of many “anti-depressant” nutrients.
The Endocrine Pathway and Stress
Stress is a digestion killer and anxiety destroys a happy gut!
Stress and rushing through meals can also affect your ability to digest your food properly. When you are stressed and busy, or not chewing your food well, your digestive organs are not getting the right signals that help them start preparing your body for the breakdown of the food.
The production of stomach acid and digestive enzymes is decreased, and this can lead to poorly digested or undigested foods sitting in the gut for longer periods, causing symptoms such as bloating, constipation, diarrhoea, reflux, inflammation, and other symptoms often linked to inflammatory bowel syndrome, or IBS, and small intestinal bacterial overgrowth, or SIBO.
Changes like these in your digestive function cause changes in the gut environment and can lead to an unhappy gut. And as we saw above, the brain will get a message about this too, and respond accordingly, and thus the food and mood connection!
And did you know that chewing impacts your brain health too, particularly the function of the brain area that is associated with memory and learning? When you eat too many soft foods, you may be harming your brain, due to decreased levels of the brain chemical called a brain-derived neurotrophic factor or BDNF. BDNF has been shown to stimulate the growth of new nerve cells and is associated with increased brain plasticity.
Food And Mood Connection - How to Create a Happy Gut and Happy Moods?
So now that you know the food and mood connection, how your gut affects your brain and how the food you eat is linked to your moods, I’m sure you are ready to take control now. So rather than letting the food you eat control your behavior and moods, you have the power to be in charge!
I’ll leave you with my top tips for a happy gut and happy you. Pick one change that you feel comfortable with and that you can do consistently every day until it becomes a natural part of your daily routine and an old unhelpful habit has been replaced by it. Then just gradually keep adding new changes to that and your gut and your brain will thank you!
Remember…
Small changes make a big difference!
My 10 Simple Hacks To a Happy Gut and Happy You!
- Reduce or eliminate refined processed foods.
- Ensure good hydration.
- Manage your stress better.
- Chew every mouthful well.
- Choose quality over quantity when buying food.
- Count colors, not calories.
- Aim for 30 different plant foods a week.
- Try some fermented probiotic foods.
- Educate your tastebuds to accept fewer sweet tastes by eating more bitter foods.
- Ensure you are eating enough good quality protein and healthy fats.
And most of all enjoy your food!
Sources
- The Lancet – Global Health Metrics| Volume 392, Issue 10159, P1789-1858, November 10, 2018. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017
- GOV.UK – Office for Health Improvement & Disparities Wellbeing and mental health: Applying All Our Health, Updated 28 February 2022 https://www.gov.uk/government/publications/wellbeing-in-mental-health-applying-all-our-health/wellbeing-in-mental-health-applying-all-our-health
- Stepping Stones Recovery College Bracknell https://www.steppingstonesrecovery.co.uk/
- Britain’s Healthiest Workplace Survey 2014-2019 https://www.vitality.co.uk/business/healthiest-workplace/findings/
- Johnson, P., Kenny, P. Dopamine D2 receptors in addiction-like reward dysfunction and compulsive eating in obese rats. Nat Neurosci 13, 635–641 (2010).
- Schulte EM, Avena NM, Gearhardt AN (2015) Which Foods May Be Addictive? The Roles of Processing, Fat Content, and Glycemic Load. PLOS ONE 10(2): e0117959.
- Lenoir M, Serre F, Cantin L, Ahmed SH (2007) Intense Sweetness Surpasses Cocaine Reward. PLOS ONE 2(8): e698.
- DiNicolantonio JJ, O’Keefe JH, Wilson WL. Sugar addiction: is it real? A narrative review. Br J Sports Med. 2018 Jul;52(14):910-913. doi: 10.1136/bjsports-2017-097971
- Liu L, Huh JR, Shah K. Microbiota and the gut-brain-axis: Implications for new therapeutic design in the CNS. EBioMedicine. 2022;77:103908. doi:10.1016/j.ebiom.2022.103908
- Bear T, Dalziel J, Coad J, Roy N, Butts C, Gopal P. The Microbiome-Gut-Brain Axis and Resilience to Developing Anxiety or Depression under Stress. Microorganisms. 2021 Mar 31;9(4):723. doi: 10.3390/microorganisms9040723.
- Breit S, Kupferberg A, Rogler G and Hasler G (2018) Vagus Nerve as Modulator of the Brain–Gut Axis in Psychiatric and Inflammatory Disorders. Front. Psychiatry 9:44. doi: 10.3389/fpsyt.2018.00044
- Costa M, Brookes SJH, Hennig GW. Anatomy and physiology of the enteric nervous system. Gut 2000;47:iv15-iv19.
- Bourassa MW, Alim I, Bultman SJ, Ratan RR. Butyrate, neuroepigenetics, and the gut microbiome: Can a high fiber diet improve brain health?. Neurosci Lett. 2016;625:56-63. doi:10.1016/j.neulet.2016.02.009
- LaChance LR, Ramsey D. Antidepressant foods: An evidence-based nutrient profiling system for depression. World J Psychiatry. 2018;8(3):97-104. doi:10.5498/wjp.v8.i3.97
- Wiertsema SP, van Bergenhenegouwen J, Garssen J, Knippels LMJ. The Interplay between the Gut Microbiome and the Immune System in the Context of Infectious Diseases throughout Life and the Role of Nutrition in Optimizing Treatment Strategies. Nutrients. 2021 Mar 9;13(3):886. doi: 10.3390/nu13030886.
- Chieh-Hsin Lee and Fabrizio Giuliani. Front Immunol. 2019; 10: 1696. doi: 10.3389/fimmu.2019.01696
- Lijuan Zhang et al. BMC Psychiatry. 2017; 17: 70. doi: 10.1186/s12888-017-1234-1
- Gara Arteaga-Henríquez. Front. Psychiatry, 09 July 2019 https://doi.org/10.3389/fpsyt.2019.00458
- Huayue Chen et al. Chewing Maintains Hippocampus-Dependent Cognitive Function. Int J Med Sci. 2015; 12(6): 502–509. doi: 10.7150/ijms.11911.

Minna Wood
Related Posts

Symptoms of SIBO vs IBS, hydrogen vs methane SIBO symptoms and Hydrogen sulfide SIBO