The Science of Nutrition for the Elderly – What is Geriatric Nutrition? Why it is important? Know the challenges of geriatric nutrition considering the various nutritional stresses among the elderly. How does the aging process affect food intake and utilization, the diseases of the elderly, and how the nutritionist help adapts low-cost foods acceptable to aging? Here are some of the low-cost food adaptation strategies and simple dietary guidelines for the science of nutrition for the elderly – geriatric nutrition! Check out this mini encyclopedia of geriatric nutrition.
What is the Science of Nutrition?
Nutrition is the science that interprets the interaction of nutrients and other substances in food in relation to an organism’s maintenance, growth, reproduction, health, and disease.
The science of nutrition includes food intake, absorption, assimilation, biosynthesis, catabolism, and excretion.
Nutrition, or the science of nutrition, can be defined as food or nourishment needed to keep an organism growing, healthy and viable.
The science of nutrition deals with nutrients, and substances ingested and necessary for the proper functioning of the body. The Science of Nutrition is a large and vital part of all the medical sciences. It has no beginning and no end.
Without adequate nutrition, there is disease, starvation, and death (WHO, 2015).
Who is a Nutritionist?
The American College of Nutrition (ACN) defines a nutritionist as “a health specialist who devotes his/her professional activity exclusively to food/ nutrition science (the science of nutrition), preventive nutrition, and diseases related to nutrient deficiencies, and the use of nutrient manipulation to enhance the clinical response to human diseases.”
The meaning of the word “Adapt”
Cambridge dictionary defines “Adapt” as to change, or to change something, to suit different conditions or uses. It also means to make suitable; to make to correspond; to fit or suit; to proportion.
To fit by alteration; to modify or remodel for a different purpose; to adjust: to adapt a story or a foreign play for the stage; to adapt an old machine to a new manufacture.
It can also be explained as making by altering or fitting something else; to producing by change of form or character: as, to bringing out a play adapted from the French; a word of an adapted form.
Definition of ‘low cost’
According to the English mobile dictionary, the word low cost means inexpensive, low-priced, economical, low, moderate, nominal, reasonable, reduced, cheap, and cut-price to be purchased or acquired at relatively little cost.
Definition of ‘Acceptable’
English mobile dictionary defines acceptable as capable, worthy, or sure of being accepted or received with pleasure.
Definition of ‘Aging’
Aging is a process of growing older. It actually begins at conception and ends at death. It encompasses the whole of life with different stages (Young age, middle age, and older age).
At all these stages, basic human nutritional needs continue but in changing patterns as we grow older.
Aging starts once growth is complete at the age of 25 years. It occurs at individual and unique gene-controlled rates.
The Aging Process – Why the need for Geriatric Nutrition?
Let us understand first the changes occurring during the aging process and why there is a need for geriatric nutrition or the science of nutrition for the elderly.
Initially, at the beginning of aging, a lot of people may not notice that it has started, and it causes no problems. Later on, these processes speed up and physiological changes become apparent. At the age of 25 years, growth seizes, and aging starts.
As we get older from 25 years, physical growth gradually declines. Loss of body cells begins, and the body tries to replace them by growing new cells depending on the nutrients available.
The gradual loss of cells at an older age leads to a reduction in the metabolism in the remaining cells, which leads to a gradual reduction in the performance capacity of most organ systems due to loss of muscle mass and strength (atrophy).
These changes – both physical and mental, vary from individual to individual and can occur rapidly in one organ system and slowly in another.
As aging continues from 70yrs and above, in general, lean body mass continues to decline and accelerates in later life. For example, by the age of 70 years, the liver loses about 25% of its weight, the kidney about 28% and the skeletal muscle diminishes by almost half, when compared with young adults. As a result of the aging process, the functional unit of the kidney (nephrons) is lost, and also due to the effect of high protein intake. Lack of physical activities also contributes to the loss of skeletal muscles.
These gradual losses of cellular units in organs result in an overall reduction in the body’s reserve capacity, thus older adults are less able to respond to environmental changes, physical stress, or conditions of diseases and infections.
Effects of aging-related changes on food intake and utilization
It is important to understand how aging affects food intake and utilization and hence nutritional challenges become important as part of the geriatric nutrition program or when understanding the science of nutrition in the elderly.
- The secretion of certain digestive juices is reduced. This can lead to indigestion of some nutrients and malabsorption of some important nutrients. Lack of gastric acid can lead to unwanted bacterial growth.
- Aging-related changes, both physical and mental, can influence the sensory perception of taste, smell, vision, and hearing although these responses are highly individualized. These senses affect appetite and the enjoyment of food and may determine the amount of food consumed.
- These changes may often lead to loss of independence and loss of self-esteem all of which can affect food intake.
- Malnutrition – Inadequate nutrient intake may result in various disease conditions which will influence the aging process
- Loss of teeth affects food intake.
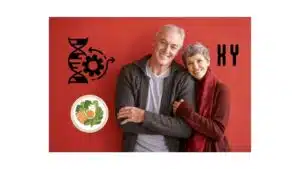
The Challenges of Geriatric Nutrition – Various nutritional stresses common among elderly
There are various nutritional stresses common among the elderly and these stresses interfere with nutrition. Hence, it is important for the nutritionist to consider these challenges in the science of nutrition for the elderly.
Stress in chewing
A large percentage of elderly people do not have all their own teeth. Some are toothless and others struggle with ill-fitting dentures. Food is therefore insufficiently chewed or kinds that require little chewing are given preference. Geriatric nutrition or the science of nutrition in the elderly may help find solutions to such challenges.
Foods that are firmer and contain a lot of food fiber, such as fruit and vegetables, are replaced by soaked bread, rusks (usually white), and other soft foods. Such food has a small volume, consequently, there is a decrease in the movement of the bowel and gut. This results in the slower passage of food along the digestive tract and gives rise to such problems as indigestion and constipation.
Loss of sense of taste and smell
The number of taste buds varies from person to person but does not decrease with age. The sense of smell gradually diminishes, which may be why some older folk lose interest in food.
Shrink salivary glands and less secretion of saliva
Normally, saliva plays an important part in the digestion of starchy foods, especially if they are thoroughly chewed and mixed with saliva. Thus, a lack of saliva can retard the digestion of starches.
When too little saliva is secreted, dry foods are not moistened properly and are therefore difficult to swallow. Consequently softer and moister foods are given preference.
Degenerated digestive tract
Less gastric acid and less of enzymes needed for digestion are secreted; intestinal motility decreases, and constipation increases. Although most of the nutrients are still well absorbed, it would nevertheless seem that the absorption of a few, such as calcium and iron, may decrease.
The choice of foods may be determined by the degree of discomfort that follows a meal. Eventually, the variety of foods tolerated by the elderly becomes so small that insufficient nutrients are ingested.
Changes in the body composition
Fat increases and muscle tissue decreases. This does not imply an increase in weight, but only a partial replacement of muscle tissue by fat. This is a normal phenomenon and should not be confused with the general but abnormal weight increase known as “middle‑age spread”.
One should remember, however, that fatty tissue is less active than muscle tissue and therefore uses up less energy. Less food will then be required to maintain the same body weight.
Decreased hormone secretion
The hormone insulin is essential to the utilization of sugar (glucose). As one grows older and less insulin is secreted, the excessive intake of sweetened food should be avoided.
Decreased Muscle coordination
This makes it difficult to manipulate eating and kitchen utensils.

Diseases of the Aged and Geriatric Nutrition
Obesity
Obesity increases the incidence and/or aggravates the discomfort of many complaints, e.g., bronchitis, shortness of breath, gallstones, hernias, and all diseases of the bones and joints (such as osteoporosis and arthritis).
Wrong eating habits sometimes play an important part in causing diseases and in some cases a change of diet forms part of the treatment. And hence the science of nutrition, geriatric nutrition, plays a role.
Constipation
One is constipated when irregular bowel movement causes discomfort and indigestion. People who have healthy living and eating habits usually have one or more motions every day. The nutritionist must consider constipation when planning a diet for the elderly as part of the science of nutrition in the elderly (geriatric nutrition).
The most common causes of constipation are:
- Too small a food residue in the intestinal tract – The volume of the residue is determined by the amount of food and liquid ingested, the amount of food fiber in the diet, and the ability of the fiber to hold water. If the food intake is small because of illness or a slimming diet the residue is, of necessity and also small.
- Neglect of the call to defecate which usually goes hand in
- Hand with living at too fast a pace and irregular toilet
- Food Habits
- Certain diseases of the digestive tract, e.g., cancer and diverticulitis (a form of inflammation occurring most frequently in the colon or large intestine); medicines such as certain painkillers and remedies containing iron can cause constipation.
- Inactivity or Immobility, when one is confined to bed, can promote constipation in one of two ways: There is a lack of adequate stimulation for the forward movement of the contents of the intestinal tract. Further, the immobile person is dependent on someone else for aid in responding to the urge to defecate. If there is no response at the right time, the urge disappears.
Hypertension
The possible causes of hypertension are:
- An inherited tendency
- Sex (men run a greater risk than women)
- Age
- Tension or Stress
- Two factors related to nutrition, viz excessive use of salt and obesity.
It is known that tension can cause a sudden and temporary rise in blood pressure.
Food that contains a lot of salt can cause hypertension in individuals with an inborn sensitivity to salt. Non‑sensitive individuals remain normal on the same diet.
The possibility of a person developing heart problems is much greater if he has high blood pressure and is, in addition, obese. A loss of weight is sometimes the only prescription for moderately high blood pressure.
Gout
Gout runs in families. It is a form of arthritis; usually, the big toe is the first joint to be affected. Individuals suffering from gout have an excess of uric acid in the blood and uric acid crystals in and around the affected joints.
Normally the uric acid is systematically excreted in the urine and only small amounts are found in the blood.
Uric acid is formed in the body from purine. The liver, kidneys, brains, gravy, meat extract, and sardines are the richest sources of purine. Other kinds of fish, all kinds of meat, dry legumes, wheat germ, and rolled oats are moderately rich sources.
Half of the uric acid in the blood of normal people is formed by the body itself. The other half, contributed by food, nevertheless plays a very important part in the control of gout and the prevention of acute attacks.
The obese should follow a diet that will reduce weight slowly. Fasting leads to an increase in blood uric acid and may bring on an attack of gout.
Diabetes Mellitus
One of the symptoms of those who suffer from diabetes is too high a blood sugar (glucose) level.
The glucose comes from digested food and is normally transported rapidly from the blood to the tissues. The ability of the elderly to handle glucose becomes impaired. The bloodstream can therefore easily become overloaded with glucose.
Diabetes which develops at an advanced age is usually of a mild nature. As a rule, no medication is necessary, as diabetes can be controlled by diet alone, and hence geriatric nutrition becomes important.
Impaired food intake
The main causes of poor food intake in the elderly/ geriatrics are:
Poor appetite
Illness, pain or nausea when eating, depression or anxiety, social isolation or living alone, bereavement or other significant life events, food aversion, resistance to change, lack of understanding linking diet and health, beliefs regarding dietary restrictions, alcoholism, reduced sense of taste or smell.
Inability to eat
Confusion, diminished consciousness, dementia, weakness or arthritis in the arms or hands, dysphagia, vomiting, chronic obstructive pulmonary disease (COPD), painful mouth conditions, poor oral hygiene or dentition, restrictions imposed by surgery or investigations, lack of help while eating for those in hospitals and rest homes.
Lack of food
Poverty, poor quality diet (home, hospital or rest home), problems with shopping and cooking, and ethnic preferences not catered for, particularly in hospitals and rest homes.
Impaired digestion and/or absorption
Medical and surgical problems affecting the stomach, intestine, pancreas, and liver, cancer, infection, and alcoholism can lead to discomfort thereby stressing the elderly.
Altered requirements
Increased or changed metabolic demands related to illness, surgery, organ dysfunction, or treatment. Excess nutrient losses: Vomiting, diarrhoea, fistulae, stomas, losses from the nasogastric tube, and other drains.
Illness related Malnutrition
Some disease states also increase the risk of malnutrition. For example, chronic respiratory, gastrointestinal, liver, and kidney diseases, cancer, HIV, AIDS, stroke, and surgery.
Surgery
The metabolic changes caused by surgery, the increased demands required for successful healing, sepsis, and the stress of the surgical procedure itself, all increase energy needs.
To supply this energy, protein stored as muscle is broken down and amino acids released. A septic state will increase this muscle breakdown further.
Cancer
People with cancer are often malnourished. Physical and metabolic changes can be compounded by social and psychological problems. These lead to adverse effects such as taste changes, nausea, or swallowing difficulties and also result in reduced food and nutrient intake.
Cancer may result in cachexic syndrome which is a state of complex metabolic changes associated with anorexia, progressive weight loss, and depletion of reserves of adipose tissue and skeletal muscle. Weight loss adversely affects treatment tolerance and survival outcomes.
Chronic Kidney Disease (CKD)
The elderly with chronic kidney disease (CKD) are prone to nausea, vomiting, edema, proteinuria, and hematuria.
These conditions pose lots of stress on them leading to nutritional stress and discomfort which can even affect their nutritional status hence the science of nutrition in the elderly or geriatric nutrition plays a significant role in such patients.
Geriatric Nutrition and Health During Older Age
Nutrition deserves special attention as people reach older age because good nutrition is essential for good health.
Healthy aging is associated with a number of physiological, cognitive, social, and lifestyle changes that influence dietary intake and nutritional status. Access to and consumption of healthy food for older people is influenced by the wider determinants of health. These determinants include cultural, social, historical, and economic factors.
A life course approach to aging recognizes that the effects of these determinants accumulate throughout the life span and have an impact on health. Because of this cumulative impact, interventions modifying the determinants of health are important at all stages of life.
Overall, good nutrition in older people is associated with:
- Preventing malnutrition
- Supporting physical function
- Reducing the risk of chronic disease
- Supporting mental health
- Preventing disability.
Many factors associated with aging affect food and nutrient intake and may promote the poor nutritional status, as also mentioned above.
Although some factors associated with age are irreversible, such as sarcopenia, dementia, etc., other factors such as food skills and knowledge, living arrangements, and the physical and social environment, are modifiable.
How do Nutritionist Adapt Low-Cost Foods that are Acceptable to the Aging as part of Geriatric Nutrition?
Food modification to suit the age, health, and challenges is an essential key in planning and preparing food that will be acceptable to the aging while still taking cognizant of their financial capability.
There are several ways nutritionists can adapt low-cost food that will be acceptable to age as part of geriatric nutrition, the science of nutrition in the elderly.
These include –
Portion size modification
If a nutritionist notices that the older adult seems to be overwhelmed by a large plate of food, for instance, they can use smaller plates or serve smaller portions, which may be more appealing.
Increase in the nutrient density
Another strategy is to increase the nutrient density of the food consumed so that every bite counts. For example, when making oatmeal, prepare it with milk rather than water.
The same approach can be taken with other foods: fruit, or protein powder to smoothies, which can also be made with milk instead of water; add gravy to potatoes or meat and sauces to a wide variety of foods; add a chopped egg to a green salad or tuna salad.
Food Texture Modification
It is necessary to modify food texture if a person has dental problems, such as loose teeth, ill-fitting dentures, impaired tongue movement, and lip closure, or problems with swallowing.
Problems with the oral processing of foods and dysphagia can be chronic and often occur simultaneously with other medical conditions.
These issues, particularly swallowing problems, can cause anxiety in caregivers, who are often concerned with providing foods that are both safe for the person to eat and enjoyed by all family members.
In this case, the nutritionist modifies the locally available foods and low-cost foods to suit the elderly. For example, food can be cooked soft and pureed. Cooked vegetables, for instance, are preferable to raw; adding gravy or sauce can help to soften and moisten foods. It may also be helpful to chop, mash, or puree food using a fork, knife, or food processor.
Remind caregivers that food needs to be appealing and tasty to ensure eating is a pleasant experience.
Geriatric Nutrition: Low-Cost Food Adaptation Strategies
The low-cost food adaptation strategies as part of geriatric nutrition include –
- Flavor foods—using pepper, herbs, and spices—based on individual preferences.
- Encourage the older adult to eat a few more bites during each meal.
- Use smaller plates and offer smaller portions.
- Choose nutrient-dense foods to make every bite count. For example:
- Use milk instead of water in oatmeal and smoothies.
- Add ice cream, fruit, or protein powder to a smoothie.
- Add gravy to potatoes and sauces to the food.
- Add chopped egg to tuna salad.
- Offer small, pre-portioned foods, such as peanut butter crackers, pudding, fruit cups, or yogurt.
Tips for adapting Food Texture
Problems to look out for includes –
- Loose teeth
- Dentures that don’t fit
- Trouble with tongue movement or closing lips to swallow.
- Coughing or choking on food or fluids.
Soft food strategies
- Avoid hard, chewy, dry, or crumbly foods.
- Cook vegetables (rather than serving them raw)
- Offer cooked cereal, pudding, mashed potatoes, scrambled eggs, yogurt, or tofu.
- Pureed food strategies.
- Puree regular or soft foods prepared for family meals in a food processor.
- Use an immersion blender to puree the solid contents of soups.
Chronic pain
- Find and treat cause wherever possible and encourage healthy eating guidelines.
Eat Healthily
- Promote low-fat and low-sugar food choices.
- Choose nourishing fluids such as milky drinks, soups, or fruit juice instead of water or tea.
- Make dessert a regular option rather than a treat.
- The Food First approach as the overall emphasis for these patients should be eating foods high in calories and protein
Thickened fluid strategies
- Make shakes and smoothies
- Add instant potato powder to thicken soups or liquids
- Use commercially available products to thicken water, juice, and broths
Managing constipation
- Increase the amount of water and fluids, up to double the usual amount of water
- Try giving half a cup of prune juice daily, followed by 60 mL of a water flush
- Increase in fruit and vegetable consumption
Maintaining hydration
- Every feeding should have a water flush before and after to make sure the tube stays open. One to two cups of additional fluids may be needed.
- A change in mental status or a fall may be an early indicator of dehydration. Other possible signs are a decrease in urine production, a furrowed tongue, a decreased amount of saliva and/or dry oral mucosa, sunken eyes, upper body weakness, a rapid pulse, and a decrease in axillary sweat production.
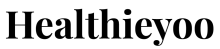
10 Simple dietary guidelines when adapting low-cost foods for the aged as part of geriatric nutrition
1. Balance food intake with the physical activity
The more active elderly are, the more food they need. Keep an eye on their meal portion size, if they are less active choose smaller serving sizes and add plenty of vegetables, salad, and fruit.
2. Include carbohydrate food at each meal
It is recommended to include carbohydrate food (bread, rice, pasta, potato, or cereal) at each meal. Choose high-fiber options whenever you can.
3. Aim for five servings of fruits and vegetables each day
Remember these servings can be fresh, frozen, tinned, or dried. Color is important. Have a mixture of different colored fruits and vegetables each day such as apples, oranges, bananas, spinach, cabbage, carrots, sweet potato, broccoli, cauliflower, peppers, and sweet corn.
4. Include Protein Foods
Protein foods help to make new cells and keep your muscles healthy. Stay fit and strong by eating a variety of protein-rich foods each day.
Great sources include lean meat, poultry, and fish. Salmon, sardines, trout, fresh tuna, and kippers are packed with heart-healthy omega-3 fats. Eating beans, eggs, and nuts is a simple way of boosting the protein in your diet.
5. Low-fat dairy foods
Keep bones healthy by having three servings of low-fat dairy foods (milk, yogurt, or cheese) each day to keep your bones healthy by having. Dairy foods with added calcium and vitamin D are even better. Look out for these in the supermarket as fortified foods.
6. Choose heart-healthy fats when planning
We all need some fat in our diet but it is a case of choosing the right type is important.
Saturated fat or animal fat
Saturated fat or animal fat can raise your cholesterol level, which can in turn increase the risk of heart disease.
Saturated fat is found in butter, hard margarine, lard, cream, cream-based sauces, fat on meat, skin on chicken, and processed meats like sausages, burgers, black and white pudding, meat pies, and pate.
It is also found in biscuits, cakes, chocolate, toffees, takeaway foods, foods covered in batter and breadcrumbs as well as milk, cheese, and yogurt.
Trans fat or hydrogenated vegetable fat
Trans fat or hydrogenated vegetable fat also raises cholesterol levels.
Trans fat is found in hard margarine, cakes, biscuits, and confectionery. It may be listed as hydrogenated fat on food labels and should be avoided.
Monounsaturated fat
Monounsaturated fat aims to replace saturated fat with monounsaturated fat to help protect your heart as it helps lower cholesterol levels.
Monounsaturated fat is found in olive oil, peanut oil, and rapeseed oil, unsalted peanuts, cashew nuts, and almonds.
Polyunsaturated fat
Polyunsaturated fat can also help to reduce cholesterol levels.
Polyunsaturated fat is found in oily fish (omega-3 fat), sunflower oil (omega-6 fat), sesame oil, flaxseed oil, walnuts, and hazelnuts.
Remember all types of fats and oils contain the same amount of fat and calories. They can lead to weight gain if used in excess.
7. Use less salt
Too much salt in the diet can contribute to high blood pressure, which in turn can lead to stroke or heart disease.
You can reduce the amount of salt in your diet by:
Avoid adding salt to your food at the table and in cooking. Use pepper, lemon juice, herbs, and spices to flavor food instead of salt.
Choosing fresh foods as often as possible e.g. fresh meat, chicken, fish, vegetables, homemade soups, and sauces without salt.
Limit intake of processed or canned food. Avoid foods high in salt such as packet and tinned soups and sauces, instant noodles, Bovril, Oxo, Marmite, stock cubes, soy sauce, garlic salt, and sea salt. Avoid processed meats such as ham, bacon, corned beef, sausages, burgers, black and white pudding, meat pies, pate as well as smoked fish.
Keep away from snacks such as salted biscuits and salted crisps and nuts. Check food labels to help you choose foods with a low amount of salt. Too much salt is more than 1.5g (0.6g sodium) per 100g of any food item.
8. Limit foods high in salt and sugar
Limit the foods high in ‘empty calories’ like biscuits, cakes, savory snacks (crisps, peanuts), sweets, and confectionery.
These foods are rich in calories, fat, sugar, and salt, so remember – not too much and not too often.
9. Dehydration
Among other things, dehydration causes tiredness, dizziness, and constipation.
Get plenty of fluids (water, fruit cordials, juice, milk) onboard each day. As a general guide, about 8 glasses a day should be adequate.
10. Alcohol
Alcohol should be enjoyed in moderation.
The recommendations are no more than 11 standard drinks a week for women or 17 standard drinks a week for men with a number of alcohol-free days in the week.
Some Important Points to Consider in Geriatric Nutrition
As we get older, our bodies have different needs, so certain nutrients become especially important for good health:
Fibre
Eating fiber-rich foods helps the bowels move regularly, lowering the risk of constipation. A high-fiber diet can also lower the risk for many chronic conditions including heart disease, obesity, and some cancers.
Good sources of fiber include:
- 100% whole meal or wholegrain bread
- Breakfast cereals such as porridge, Weetabix, shredded wheat, and bran flakes
- Other cereals such as brown rice, brown pasta
- Potatoes eaten in their jackets
- Fruits and vegetables, Pulse vegetables such as beans, peas, and lentils
- Breakfast can be a super way to get a high-fiber start to the day: Add linseed to a wholegrain cereal or to yogurt or have prune juice instead of orange juice to boost your fiber intake.
Calcium and Vitamin D
Older adults need extra calcium and vitamin D to help maintain bone health.
Being a healthy weight can help keep bones strong.
Take three servings of vitamin D-fortified milk, cheese, or yogurt each day.
Other calcium-rich foods include fortified cereals, dark green leafy vegetables, and canned fish with soft bones (like sardines).
Iron and Vitamin B12
Iron is responsible for carrying oxygen around the body, while vitamin B keeps your brain and nervous system healthy.
Many older adults do not get enough of these important nutrients in their diet.
The best sources of iron include red meats such as beef, liver, kidney, lamb, pork, ham, corned beef & black & white pudding, while fortified cereals, lean meat and some fish and seafood are sources of both iron and vitamin B.
Taking vitamin C-rich food like orange juice at mealtime can help your body to absorb iron.
Exercise and Active Lifestyle
A word on exercise combining an active lifestyle with a healthy diet is your best recipe for healthy aging.
Try to be physically active for at least 30 minutes most days. It is okay to break up your 30-minute physical activity into 10-minute sessions throughout the day.
If you are currently inactive, start with 5 minutes of exercise, such as walking, gardening, climbing stairs, or dancing, and gradually increase this time as you become stronger.
Conclusion
Food modification to suit age, health, and challenges is an essential key in planning and preparing food that will be acceptable to the elderly while still taking cognizance of their financial capability.
There are several ways nutritionists can adapt low-cost foods that will be acceptable to aging.
It is necessary to modify food texture if a person has dental problems, such as loose teeth, ill-fitting dentures, impaired tongue movement, and lip closure, or problems with swallowing.
Problems with the oral processing of foods and dysphagia can be chronic and often occur simultaneously with other medical conditions. These issues, particularly swallowing problems, can cause anxiety in caregivers, who are often concerned with providing foods that are both safe for the person to eat and enjoyed by all family members.
Nutrition deserves special attention as people reach older age. Healthy aging is associated with a number of physiological, cognitive, social, and lifestyle changes that influence dietary intake and nutritional status. Geriatric nutrition is the science of nutrition that takes care of the above-mentioned challenges in the elderly.
References
- World Health Organisation (2015). Nutrition for health and development (NHD). Progress and prospects on the eve of the 21st century. Geneva: World Health Organization.
- https://www.encyclopedia.com/
caregiving/encyclopedias- almanacs-transcripts-and-maps/ nutritionist-definition#:~: text=The%20American%20College% 20of%20Nutrition,clinical% 20response%20to%20human% 20diseases - https://www.merriam-webster.
com/dictionary/acceptable - https://www.collinsdictionary.
com/dictionary/english/low- cost

Dietitian Obianuju A Orjiekwe - Ezenkwele
Related Posts

Healthy Aging Month 2022: You Are The “Driver” Of Your Health And Wellness
Healthy Aging Month 2022! September is designated as Healthy Aging Month! Let us celebrate healthy aging month 2022 and imbibe some real healthy aging
How Does Nutrition Affect Longevity And Gene Expression?
Diet and Gene Expression – How does nutrition affect longevity and gene expression? Can diet change your genes? Can diet or nutrition affect longevity

Multivitamin, Probiotic, Omega 3 – Don’t Let Dietary Supplement Selection Overwhelm You
You’re here. You have finally decided to take control of your health and are looking into which dietary supplement to add to your wellness toolbox.
Improving resistance, resilience, and recovery from COVID-19 through personalised nutrition and lifestyle interventions
A holistic element of improving resistance, resilience, and recovery from long Covid through personalised nutrition and lifestyle interventions is described here highlighting five specific focus

10 Strategies for Leveraging Active Aging in Covid-19
Know the activity theory of aging and its importance during the pandemic. Here are the 10 strategies for leveraging active aging in COVID-19. THE PROBLEM

Approaching 40, 50? This is how you can stay healthy!
Are you approaching your 40 or 50? This is how you can stay healthy! Read on! As you age, your VO2 Max starts declining by 10%