Chronic Kidney Disease, CKD & Bone disease –
“I want to have strong bones, but my labs keep showing that my calcium level is low. Should I start drinking more milk?” – CKD Patient

Everyone wants strong bones. Who doesn’t? In fact, osteoporosis (a disorder of decreased bone strength) affects 10-12 million people in the U.S. alone. Since the #1 risk factor is age, this is becoming an increased concern as the worldwide population ages rapidly. Worried about breaking a bone? Well, consider this… the fracture rate for someone with chronic kidney disease (CKD) is the same as for someone without CKD who is 10-20 years older. Given that CKD is an independent risk factor for bone disease, and that the median age of a dialysis patient is 60 years, bone health should be a top priority for this population.
A little background on Calcium
Calcium is the most abundant mineral in the body which is needed to build and maintain strong bones and teeth. Calcium is also needed to regulate nerve, cardiovascular and hormonal function. 98% of total body calcium is in the bones. The other 2% circulates in the body.
The renal dietitian (RD) will sometimes look at “Corrected Calcium” which is calculated to account for the Calcium attached to Albumin, the primary blood protein. It is most helpful in patients with low Albumin. Corrected Calcium = Serum Calcium + (4-Albumin X .8).
What is Bone Mineral Disorder (BMD) in Chronic Kidney Disease?
Bone Mineral Disorder (BMD) is a disorder among people with chronic kidney disease (CKD) that affects the bones, heart, and blood vessels. When the kidneys stop filtering and regulating hormones normally, calcium and Phosphorus attach to each other and form deposits. These deposits can cause clotting in the vessels as well as loss of bone mass leading to bone disease in CKD patients.
As the bones lose these key minerals, they become weak and are subject to fracturing, breaking, or deformities.
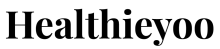
Below are the most common risk factors for bone fractures or bone disease or bone mineral disorder in chronic kidney disease or CKD patients.
Risk Factors for Bone Fractures in people with CKD
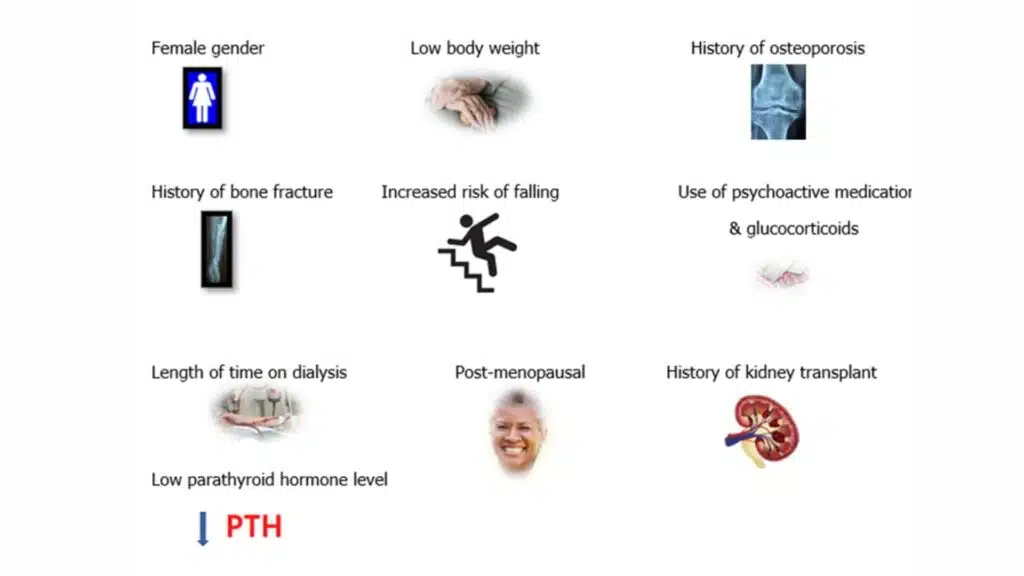
Both low and high levels of Calcium are cause for concern depending on how high and how low they are. Generally, 7.5-8.2 mg/dL is considered mildly low, and a nephrologist may not choose to add any Vitamin D or calcium supplement within that range. A calcium level between 10.2-11.0 mg/dL may also not cause too much concern depending on a doctor’s interpretation of the lab. However, most renal RD’s will work to find out the best way to bring calcium within normal limits (see Table 1)
High Calcium
In the general population, the most common reasons for high calcium levels (hypercalcemia) are primary hyperparathyroidism and malignancy. In Chronic kidney disease (CKD) patients, the primary reason is secondary hyperparathyroidism.
High Calcium levels, when seen in CKD patients, may also be an indication of dehydration, excessive doses of Vitamin D and/or calcium supplementation, low mobility (i.e. wheelchair-bound or bedridden), tertiary hyperparathyroidism, and malignancy.
- Primary hyperparathyroidism is mainly caused by a non-cancerous tumor on or overgrowth of the parathyroid glands.
- Secondary hyperparathyroidism starts with the kidneys’ inability to convert Vitamin D to its active form. Calcium levels then begin to go down due to low absorption. This can cause the parathyroid hormone (PTH) gland to grow larger and secrete excess hormones.
- Tertiary hyperparathyroidism results from prolonged high Phosphorus levels and low Vitamin D levels leading to increased secretion of PTH.
- In all cases, stimulation of PTH raises calcium by bone resorption (breaking down bone) and increasing calcium resorption (decreasing excretion of calcium) from the kidneys.
- Hypercalcemia is associated with low bone turnover and is prevalent among those on peritoneal dialysis.
Low Calcium
Low Calcium levels are much more common in CKD patients than high Calcium. Usually, the cause of low calcium is insufficient active Vitamin D (Calcitriol). Since normal working kidneys activate Vitamin D (in food) to a form that the bones can use, most people with CKD need to take activated Vitamin D to maintain normal calcium levels.
Some Myths
Myth: “Low blood calcium means that I don’t have enough Calcium in my body to make strong bones”.
Answer: Not exactly. Low Calcium in the presence of CKD is usually due to insufficient activated Vitamin D. Since Vitamin D is required for the absorption of Calcium, low Vitamin D levels can cause low serum calcium. Therefore, your body, with diet may contain enough Calcium and you may just need an activated Vitamin D supplement to increase calcium levels.
Myth: “I am a man with big bones, I am not really at risk for bone disease or fractures”.
Answer: Not really. Although women are generally at a higher risk (post-menopause) for bone disease, the size of a person’s bones, especially with CKD, does not lessen the risk. In fact, excess body weight (BMI over 30) can contribute to increased stress on the bones leading to fractures.
Myth: “I am too old to exercise. I am too tired and my bones and joints ache”.
Answer: Actually, exercise is one of the best ways to improve bone density. Exercise can also help decrease excess body fat to help relieve extra pressure on your joints. Bones and joints were meant to move for these reasons as well as to maintain proper blood flow. Fatigue and achy joints may actually be a symptom of not enough exercise.
Myth: “The higher my Calcium level is, the healthier my bones will be.”
Answer: People with CKD, according to KDIGO guidelines, should strive to maintain calcium levels below 10.5 mg/dL. Furthermore, it is recommended that the use of calcium-containing Phosphorus binders should be “restricted”. There is no established limit on how much Calcium should be consumed among those with CKD, however, general practice has been to limit to not more than 1500 mg/day. Although, a positive calcium balance (high calcium) has been found with Calcium intake as low as 800-1000 mg/day in some studies.
Myth: My regular doctor (PCP) suggested I take extra Vitamin D to help my overall health and prevent COVID infection.
Answer: Improving Vitamin D levels when they are low (under 30 ng/mL) is recommended for most people. CKD patients should always inform their kidney doctor about any extra supplement, including Vitamin D. Extra Vitamin D may cause higher than recommended calcium levels which can be toxic as well as promote calcifications in your blood vessels. Although Vitamin D is considered an antioxidant giving anti-inflammatory benefits, it has not been proven to prevent infection or be an effective treatment for COVID-19 infection.
Myth: Milk is a good source of both Calcium and Vitamin D. Can I just start drinking that?
Answer: Well, kind of… Milk is a good source of Calcium and when fortified with Vitamin D, may contain up to 25% of the recommended daily value. However, for CKD patients, milk is generally restricted due to its high Phosphorus content. There are certain milk-based protein shakes made specifically for CKD/dialysis patients which are formulated to be low in Phosphorus. Blood Phosphorus levels must be maintained within normal limits to avoid Phosphorus-Calcium deposits which is the number one cause of calcifications leading to amputations, stroke and heart attack in this population.
How much Calcium do I need?
Adults aged 19-50 are recommended to consume at least 1000 mg of Calcium/day. Men aged 51 and over are recommended the same amount while women in this age group are suggested to have at least 1200 mg/day. These amounts are slightly higher for teenagers and during pregnancy. Having CKD does not change these amounts significantly and is best determined by your doctor and dietitian. Calcium intake above 2000 mg/day can be harmful to older adults by increasing the risk for heart disease.
Certain groups of people are at higher risk of not getting enough calcium in their diet and therefore increases the risk of bone disorder:
- Children aged 4-18 years
- Black/African American and Asian
- Age 50 and older living in poverty
- Post-menopausal women
- People who are lactose intolerant
- People who follow a vegan diet (no animal products)
What are the best sources of calcium?
Calcium is found in high amounts in the following categories of foods:
- Milk, milk products such as cheese and yogurt
- Fish (especially salmon, tuna, and sardines with the bones)
- Dark green vegetables such as kale, broccoli, and cabbage
- Fortified cereals, juices, and milk substitutes

If you are living with CKD, a dietitian can help determine which of these foods would be safe as it depends on the stage of the disease and if on dialysis, the type of dialysis. Many foods high in Calcium are also high in both Potassium and Phosphorus, making it a little tricky to manage.
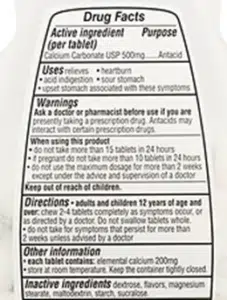
Calcium, in the form of a supplement, can be helpful especially for those with CKD to eliminate the extra minerals which the kidneys are not filtering well. Calcium supplements come in the form of Calcium Carbonate and Calcium Citrate. Calcium Carbonate is best absorbed when taken with food. The Citrate version is absorbed with or without food.
Calcium supplements should be taken in 500 mg or less at a time. Antacids are often prescribed by nephrologists to kidney patients as a calcium supplement. When using antacids, note that the calcium content in some antacids is different from the milligrams on the label. (Ex. Tums 500 mg contains 200 mg Calcium).
Declining kidney function is associated with age based on the U.S. NHANES III survey data indicating that of those over age 70, only 26% had normal kidney function. 49% (about half) had mildly decreased function. The number of persons aged 65 and older is expected to rise to 72 million by 2030 (32 million in 1990) and the global population reflects a similar rise in numbers. Considering these trends, kidney health is an area primary care doctors will need increased focus on by screening for CKD.

Cheryl Robinson
Related Posts

Prostadine Reviews: Unlocking the Potential for Prostate Health


Local Delicacies: A Path to Combat the Surge in Non-Communicable Diseases