Gut microbiome imbalances can cause dysbiosis and pain, including that of osteoarthritis. Support a healthy gut microbiome through diet!
What is the role of the Gut Microbiome?
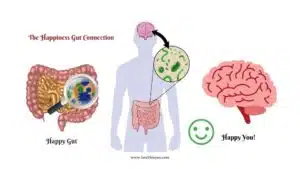
What if there were trillions of little bugs living inside of us that impacted our pain, inflammation, brain function, mood, and metabolism? This is not science fiction but how our bodies work. We live in symbiosis with these bugs. Our bodies host trillions of different microorganisms including bacteria, viruses, fungi, and parasites.
The Gut Microbiome is the collection of diverse microorganisms that live in the gastrointestinal tract. The type, size, and function of this diverse and large group of microorganisms varies. The sheer volume is outstanding with bacterial cells outnumbering human cells. In some ways, we are a walking ecosystem. The gut flora shape how we process food, interact with our environment and build health. Gut flora is involved in joint health, inflammation levels, processing vitamins, immune function, brain function, mood, metabolism, and weight gain. This impacts our mind and body on multiple levels.
The gut communicates with organ systems throughout the body. For example, the gut-brain axis connects the GI nervous system, vagus nerve, immune system, hormone signals, and gut bugs. This two-way street impacts our mood and pain tolerance. Imbalances of this axis lead to an inflammatory response in the brain and spinal cord called neuroinflammation. This leads to brain fog, headaches, and decreased pain tolerance, and is a common factor in neurodegenerative diseases such as Alzheimer’s and Parkinson’s diseases. Our gut health matters and shapes our daily function as well as our pain levels.
Several factors shape our gut microbiome including our individual experiences, environment, and stressors. Studies of identical twins have found significantly different gut microbiome compositions. Gut health rests on a number of environmental factors and encounters. In fact, the gut microbiome is influenced by birth our delivery mode (vaginal or C-section), and other factors including breastfeeding, geographical location, and contact with family members. The beauty of these external factors impacting our gut microbiome is that we can work to improve it. It is dynamic and we have the power to cultivate a healthier gut.
Gut Microbiome Imbalances: Dysbiosis & Pain
The gut microbiome is a thriving system and the primary bacteria phyla are Firmicutes and Bacteroides. They are involved in our nutrition, defense, and immune responses. They impact our metabolic function and brain health. If supported and well-fed with dietary fiber, gut bacteria create short chain fatty acids such as butyrate, propionate, and acetate to support the intestinal barrier and immune function.
Butyrate acts as an energy source for intestinal cells and is the first line of defense against pathogens. It also supports regulatory T cells (Treg) that suppress inflammation and prevent the production of inflammatory cytokines. This helps us regulate our inflammatory response and reduce ongoing systemic inflammation and pain. We must support our beneficial bacteria to thrive.
Dysbiosis is an imbalance in the gut microbiome that can be caused by less microbiota diversity, less beneficial microbiota bacteria, or more harmful microbiota. This imbalance disrupts the gut homeostasis and contributes to disease. The Standard American Diet (SAD) triggers dysbiosis. It is loaded with processed food, added sugar, excess salt, unhealthy fats, and artificial ingredients while devoid of vegetables and fruits. This nutrient-poor diet is sad and making us sicker. In fact, the 2022 task force report on Hunger, Nutrition, and Health recommended that the White House support “Food is Medicine” health initiatives. It is clear that our food choices impact our health, function, and longevity. What we feed our gut matters for our overall health, joint health, and pain control. Poor gut health in the form of dysbiosis leads to more inflammation and pain.
Table 1. Common Causes of Dysbiosis
High sugar and high unhealthy fat diets such as the Standard American Diet
Medications such as excess antibiotics and antacids
Stress, Infections, Aging
Food additives, artificial sweeteners
Dysbiosis has been associated with allergies, autoimmune disease, diabetes, cancer, and joint conditions through altered immune response and increased whole-body inflammation. Increased joint inflammation manifests as pain, heat, redness, swelling, and loss of function. Dysbiosis promotes whole-body, systemic inflammation and local joint inflammation. In a dysbiotic state, certain gut bacteria release pro-inflammatory lipopolysaccharides (LPS). Higher blood levels of LPS correlate with higher joint fluid levels of LPS and more inflammation, pain, bone spurs, and significant arthritis. A gut microbiome imbalance from unhealthy diets such as high-fat, high-sugar, and low-fiber leads to a rise in LPS, shift in types of gut bacteria, and is associated with more osteoarthritis. Studies have found a loss of microbial diversity, decrease Bacteriodes population, and increase in Streptococcus species contribute to the development and progression of osteoarthritis. This results in the production of more pro-inflammatory signals and less anti-inflammatory signals.
An unbalanced gut microbiome correlates with chronic musculoskeletal pain. This includes conditions such as fibromyalgia in which recent studies have suggested a combination of gut dysbiosis, neuroinflammation, and sarcopenia drive the disease process. The overall increase in inflammation drives disease and pain. A 2023 article in The Journal of Clinical Orthopaedics and Trauma notes the connection between gut dysbiosis and orthopaedic conditions including spinal disc conditions with recommendations to consider treating the gut in the management of orthopaedic conditions. Unfortunately, current treatments for musculoskeletal pain, back pain, joint pain, and arthritis primarily target the symptoms without addressing the causes such as gut health. We can reduce inflammation by improving our nutrition, activity level, and stress levels while being mindful of medication use. This starts by feeding the beneficial bacteria with prebiotic foods and increasing the beneficial bacteria population with probiotic foods.
How to Support a Healthy Gut Microbiome?
An optimal microbiome helps us digest food, absorb vitamins, fight infections, and lower painful inflammation. An unbalanced gut microbiome creates chaos, dysfunction, and pain. The SAD directly affects the “gut-joint axis” and leads to more swelling, more inflammation, more pain, and more dysfunction. It lacks plant-based prebiotic and probiotic foods that support gut health and joint health.
Prebiotic foods feed the beneficial bacteria such as onions, apples, asparagus, artichokes, cabbage, almonds, leeks, flaxseeds, seaweed, and leafy greens. A 2021 review study on the gut microbiome and osteoarthritis noted plant sugars such as fructo-oligosaccharides (FOS) are prebiotics that remain undigested until they reach the colon and then, feed the beneficial bacteria. This supports gut and joint health unlike a high-fat diet, a high-sugar diet, and obesity which disrupt the gut balance. Diet can have a large impact on gut and joint health.
In addition to prebiotic foods, probiotic foods improve gut health. They contain beneficial bacteria such as cultured and fermented foods including plain, unsweetened yogurt, kimchi, sauerkraut, pickles, miso, and tempeh. Positive daily choices can impact long-term gut and orthopaedic health. The first pillar of my Relief-5R plan, Refuel, improves our food intake for better gut health and less painful inflammation. It is based on taking tiny steps that add up to big health results. I call these little tweaks, microboosts. Here are some general microboosts to better support your gut health and overall health.
Table 2. General Microboosts for Gut Health & Orthopaedic Health
Stay hydrated with water and skip sodas and juices
Eat high-fiber vegetables and fruits including prebiotic and probiotic foods
Eat more fermented foods which support a healthy gut microbiome
Avoid foods with added sugar and artificial ingredients
Practice a daily, stress-relieving activity for 10-15 minutes
Avoid long-term use of non-steroid anti-inflammatories (NSAIDs)
Stay physically active and move more throughout the day
The bottom line is to focus on vegetables, high-fiber fruits, unprocessed foods, and fermented foods for a balanced microbiome. While most people do not receive prescriptions for health-promoting and pain-fighting foods, they should. What we put on our plates and feed our gut makes a big difference!
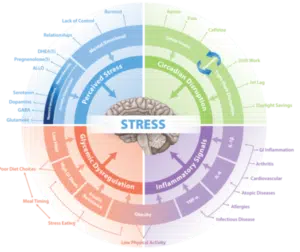
Beyond food, other daily lifestyle medicine choices impact our gut and overall health. The complete Relief-5R plan is Refuel (nutrition), Revitalize (movement), Recharge (restorative sleep), Refresh (stress management and mindset), and Relate (relationships and purpose). This is evidence-based wellness, simplified for you.
Revitalize focuses on adding more movement to our day to prevent muscles loss, boost mood, and prevent blood sugar spikes.
Recharge helps cultivate quality sleep to support cellular clean-up (autophagy) and prevent the build-up inflammatory, zombie cells.
Refresh teaches the importance of mindset and practical ways to break the stress cycle and activate the parasympathetic relaxation response.
Relate delves into the supreme importance of supportive social connection and a sense of purpose.
Together this plan empowers you to live better with greater gut health, less pain, less inflammation, and more joy. It starts with little steps and improving our gut health. If we take care of our beneficial gut bacteria, they will help take care of us. We have the power to thrive and take back control of our health. For your own personalized Relief-5R plan, explore the book The Pain Solution: 5 Steps to Relieve and Prevent Back Pain, Muscle Pain, and Joint Pain without Medication.
Cheers to supporting gut health, reducing pain, and living better!
Sources
1.Ursell, L.K., et al. Defining the Human Microbiome. Nutr Rev. 2012 Aug; 70(Suppl 1): S38–S44.
2. Sender, Ron, Shai Fuchs, and Ron Milo. “Are we really vastly outnumbered? Revisiting the ratio of bacterial to host cells in humans.” Cell 164.3 (2016): 337-340.
3. Makdissi, Stephanie et al. “Towards early detection of neurodegenerative diseases: A gut feeling.” Frontiers in cell and developmental biology vol. 11 1087091.
4. Goodrich, Julia K., et al. “Human genetics shape the gut microbiome.” Cell 159.4 (2014): 789-799.
5. Milani, Christian et al. “The First Microbial Colonizers of the Human Gut: Composition, Activities, and Health Implications of the Infant Gut Microbiota.” Microbiology and molecular biology reviews : MMBR vol. 81,4 e00036-17.
6. Schulthess, Julie et al. “The Short Chain Fatty Acid Butyrate Imprints an Antimicrobial Program in Macrophages.” Immunity vol. 50,2 (2019): 432-445.e7.
7. Informing the White House Conference on Hunger, Nutrition, and Health. Task Force Report 2022. Accessed April 29, 2023. https://informingwhc.org/2022-task-force-report/
8. Hrncir T. Gut Microbiota Dysbiosis: Triggers, Consequences, Diagnostic and Therapeutic Options. Microorganisms. 2022;10(3):578.
9. Gleason B, Chisari E, Parvizi J. Osteoarthritis Can Also Start in the Gut: The Gut-Joint Axis. Indian J Orthop. 2022 Mar 16;56(7):1150-1155. doi: 10.1007/s43465-021-00473-8.
10. Favazzo LJ, Hendesi H, Villani DA, et al. The gut microbiome-joint connection: implications in osteoarthritis. Curr Opin Rheumatol. 2020;32(1):92-101.
11. Guido G, Ausenda G, Iascone V, Chisari E. Gut permeability and osteoarthritis, towards a mechanistic understanding of the pathogenesis: a systematic review. Ann Med. 2021 Dec;53(1):2380-2390.
12. Szychlinska MA, Di Rosa M, Castorina A, Mobasheri A, Musumeci G. A correlation between intestinal microbiota dysbiosis and osteoarthritis. Heliyon. 2019;5(1):e01134.
13. Gregory Livshits, PhD, Alexander Kalinkovich, MD, PhD, Specialized, Pro-Resolving Mediators as Potential Therapeutic Agents for Alleviating Fibromyalgia Symptomatology, Pain Medicine, Volume 23, Issue 5, May 2022, Pages 977–990, https://doi.org/10.1093/pm/pnab060
14. Jeyaraman, Madhan, Arulkumar Nallakumarasamy, and Vijay Kumar Jain. “Gut Microbiome-Should we treat the gut and not the bones?.” Journal of Clinical Orthopaedics and Trauma 39 (2023): 102149.
15. Chisari E, Wouthuyzen-Bakker M, Friedrich AW, Parvizi J. The relation between the gut microbiome and osteoarthritis: A systematic review of literature. PLoS One. 2021;16(12):e0261353.

Dr. Saloni Sharma, MD
Related Posts
How To Have A Happy Gut For A Happy You!
Food And Mood Connection and the happiness gut connection – Did you know that happy foods lead to happy moods via a happy gut? Mental

Symptoms of SIBO vs IBS, hydrogen vs methane SIBO symptoms and Hydrogen sulfide SIBO
SIBO – the real cause of your bloating and how to get rid of it? SIBO stands for Small Intestinal Bacterial Overgrowth and is one

Women And Gut Health: Its Impact On Periods Health
Gut health, it’s this sexy term that is thrown around in our culture today but what does this term truly mean? Well, I’m going to
Synbiotic, Prebiotic, Probiotic – Take Care Of Your Gut
What is Gut Microbiota? Why do we have Gut Microbiota? What is Dysbiosis? What are dysbiosis symptoms? What causes dysbiosis? How to maintain a healthy
Improving resistance, resilience, and recovery from COVID-19 through personalised nutrition and lifestyle interventions
A holistic element of improving resistance, resilience, and recovery from long Covid through personalised nutrition and lifestyle interventions is described here highlighting five specific focus

Skin Microbiome and Bathing – Best Soap for Skin Miicrobiome?
Bathing and Your Skin Microbiome Recently, a debate among Hollywood celebrities emerged on whether people should bathe as little as possible (1). While some